Food Allergy: How to Care for Your Child
When someone has a food allergy, their infection-fighting immune system overreacts to proteins in the food. If the person eats this food, called an allergen, the body thinks these proteins are harmful invaders and works to fight off the invader. This causes an allergic reaction.
Allergic reactions can cause symptoms in different parts of the body, such as the skin, lungs, and digestive tract. Some reactions may be mild and just lead to one symptom, like hives. Others can be more severe. A severe allergic reaction is called anaphylaxis. Anaphylaxis can begin with some of the same symptoms as a mild reaction, but then can quickly get worse.
Symptoms of anaphylaxis may include:
-
trouble breathing, swallowing, or speaking
-
tightness in the throat
-
swollen tongue or lips
-
a hoarse voice
-
wheezing
-
coughing
-
vomiting
-
feeling lightheaded or fainting
-
many hives on different parts of the body or widespread redness
-
a combination of two mild symptoms, like a few hives with nausea
Even a child who has had a mild reaction in the past can have anaphylaxis in the future.
Epinephrine is a medicine that treats anaphylaxis. Your child should use an epinephrine auto-injector right away if having any symptoms of a serious allergic reaction.
By avoiding the food your child is allergic to and being prepared, you can help keep your child safe.

-
Follow the list of foods to avoid that the health care provider gave you.
-
Read food labels carefully every time you give a food to your child:
-
Double-check labels. Food companies change ingredients from time to time. So ingredients in a new package may be different from ingredients in an older package.
-
Look for the "top 8" allergens. The 8 most common food allergens are milk, soy, egg, wheat, peanuts, tree nuts, fish, and shellfish. U.S. law requires that these "top 8" be listed on food labels by their commonly known name.
-
Remember that many allergens aren't listed by name. If your child is allergic to foods other than the "top 8," these other foods could be hidden in ingredients like "natural flavors" or "spices." If you have any questions about whether a product contains an allergen, call or email the company.
-
Look for cross-contamination. Some foods look OK from the ingredient list, but while being made might have come in contact with a food your child is allergic to. Avoid products in packages with words such as "may contain," "processed in a facility that also processes," or "manufactured on equipment also used for" if they include your child's allergen. Only some companies label for possible cross-contamination, so call or email the company with any questions.
-
Before your child eats or you prepare food, wash hands well with soap and water. Hand sanitizing gel doesn't get rid of allergens. If soap isn't available, hand cleaning wipes can be used.
-
If you decide to keep foods that your child is allergic to in the house, keep allergen-free foods separate. Always clean utensils well before using them for allergen-free foods.
-
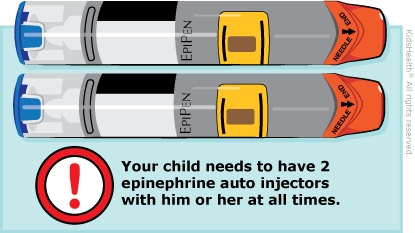
Always be prepared for a reaction. Your child should have two epinephrine auto-injectors available at all times, including at school, child care, and activities. This is in case one injector does not work or your child needs another dose of epinephrine before help arrives in an emergency.
-
Make sure the epinephrine auto-injectors have not expired. Avoid exposure to extreme temperatures (too hot or too cold) and sunlight. All caregivers should know how to use the auto-injector. Talk with your health care provider about how to recognize the signs of an allergic reaction.
-
Ask the health care provider for a food allergy action plan. Then:
-
Discuss your child's food allergy with teachers, the school nurse, and any other care providers. Share the action plan with them and develop a plan for snacks, lunch, art projects, field trips, and other risky situations. Be sure they know how to respond to an allergic reaction.
-
Your child should always wear a medical alert ID bracelet stating his or her name and allergies. You can buy one in a drugstore or online.

If your child shows signs of anaphylaxis, such as trouble breathing, throat tightness, a combination of two mild symptoms (such as hives with vomiting), or loss of consciousness, follow these steps, in this order:
-
Give your child the epinephrine auto-injector right away. Give the epinephrine even if you're not sure your child needs it. It won't do any harm. After getting the epinephrine, your child must go to the ER to see if any other treatment is needed. This is true even if your child is doing better, because there can be a second wave of symptoms.
-
Call 911.
-
If someone is with you, have that person call 911 and tell the person your child is having a life-threatening emergency.
-
If you're alone, give epinephrine first, then call 911 right away and say your child is having a life-threatening emergency.
-
Lay your child down with the legs raised while you wait for the ambulance.
-
Don't take your child to the ER in a car. Wait for an ambulance with trained specialists to transport your child.
-
Take the used epinephrine auto-injector to the hospital with you.

What should I consider when my child with food allergies goes to school? Depending on your child's age, you may want to ask school staff about:
-
where your child will eat
-
who will clean the table
-
who oversees lunchtime and snack time
-
who will be responsible for hand washing
-
who will train substitute teachers and special-subject teachers to recognize and treat a reaction
-
where epinephrine will be kept and who should give it, if needed
-
discouraging food sharing among all children
-
getting several days' notice of food-related events, including birthday parties
Look out for non-food items that could contain allergens, such as materials for art, class projects, or class pets and their food.